Abstract
Background. A Deep Molecular Response (DMR), defined as BCR-ABL1 p210 transcript at levels <= 0.01% by QPCR, is the prerequisite for a successful interruption of treatment in patients with CML. However, approximately 50% of patients in Treatment Free Remission (TFR) studies had to resume therapy after BCR-ABL1 p210 transcript levels rose above the 0.01% DMR threshold. To improve transcript detection sensitivity, transcript levels were analyzed using D-PCR. D-PCR increased BCR-ABL1 transcript detection sensitivity by 10-100 fold, however its ability to better select successful TFR patients remains unclear. Beyond the role of the immune system, relapse may be due to the presence of residual leukemic stem cells (LSCs) that are transcriptionally low or silent, insensitivity to tyrosine kinase inhibitors (TKIs) or other CML-causing transcripts not easily detectable by BCR-ABL1 PCR techniques Another approach is to use flow cytometry to detect and quantify bone marrow Ph+ LSCs CD34+/CD38− that co-express CD26 (dipeptidylpeptidase-IV) although its meaning in TFR is unclear.
Aim. To compare and examine values of the three different methods of detecting minimal residual disease (MRD) in CML at RNA and LSC levels in patients in TFR or DMR.
Patients and Methods. The twenty-seven patients in this study received treatment with either Imatinib (12), Dasatinib (6), Nilotinib (7), Bosutinib (1) or Interferon (1). Twelve patients were in TFR, while the rest were in DMR. TFR patients had stopped therapy for less than 1 year (3), <3 years (2), 6 years (6) and 17 years (1). Blood samples were collected and tested 3 times. BCR-ABL1 transcript quantification was performed using the automated Xpert Ultra BCR-ABL1 MonitorTM Cepheid method and calibrated for the ABL reference gene and BCR-ABL1 target gene. Samples were analyzed according to the manufacurer with results expressed in BCR-ABL1/ABL %IS, or undetectable transcript (U), with PCR sensitivity of 5.0 (>250,000 ABL copy numbers).
D-PCR analysis used TaqMan-MGB probes targeting the BCR-ABL1 transcript. A custom assay was designed and produced with a FAM-label, basing on the sequence of routinely-used probes. BCR-ABL1 quantifications were performed analyzing 50ng of cDNA on a QuantStudio 3D Digital PCR System (ThermoFisher Scientific). BCR-ABL1 transcript values using dPCR were expressed as number of copies/ul. The secondary analysis were carried out by AnalysisSuite Cloud Software (ThermoFisher Scientific).
To detect peripheral blood circulating CD34+/CD38-/CD26+ LSCs, cells were incubated with anti-CD45 (BD Biosciences), anti-CD34 (581), anti-CD38 (HIT2) and anti-CD26 (M-A261) (BD Pharmigen). Acquisition and analysis were performed by FACSCanto II flow cytometer (BD Biosciences, NR Nannini). CD45+ cells acquired for each sample ranged from 500,000 to 1,000,000. Isotype controls were included in each staining. Median absolute number of CD26+ cells/μL were calculated as follows: (# WBCs/μL) × (% CD34+/CD38−/CD26+ stained CD45+ cells).
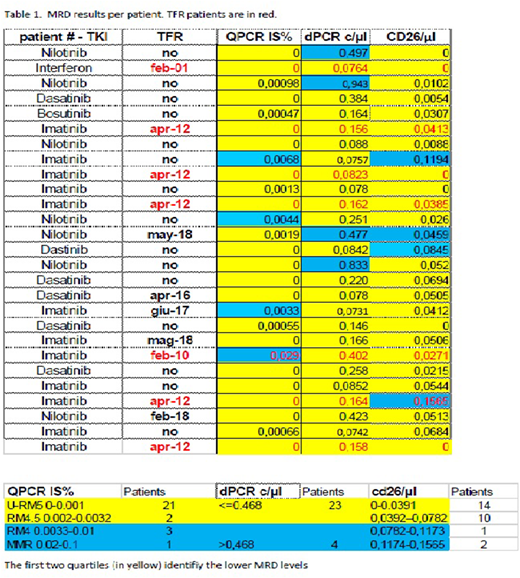
Results. TFR status, the type of TKI treatment, QPCR results, dPCR data and LSCs quantification are summarized in Table 1.
Both d-PCR and LSCs showed higher sensitivity than QPCR, exhibiting positive results when transcript levels using QPCR were undetectable (16). None of the patients tested negative with d-PCR, however 14/16 were under the threshold of 0.468 copies/uL, corresponding to a stable DMR. LSC levels were negative in 5 patients, 3 of which also tested negative with QPCR. In all patients QPCR ranged from 0-0.0068, d-PCR from 0.073 to 0.943, and LSCs from 0 to 0.156.
Results were divided in quartiles, depending on molecular response for QPCR, the 0.468 threshold for dPCR and the distribution for the LSCs. The 2 lowest quartiles defined the lowest detectable DMR. A strong correlation of these data in TFR patients was noted (10/12 concordant) while 8/15 DMR patients were discordant.
Conclusions To our knowledge this is the first attempt to analyze and compare DMR in a CML population using standard (QPCR) and highly sensitive (dPCR and LSCs) methods. TFR patients, some lasting up to 17 years, were in the lowest detectable DMR categories. Very little is known about the biology of CML implications of circulating LSCs. Larger studies and dynamic scoring will help define their informative and predictive value.
Abruzzese:Pfizer: Consultancy; Ariad: Consultancy; Novartis: Research Funding; BMS: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal